News and Updates
Navigating your dental visit: Get the expert’s take with Dr. Paul Bhatti, OTIP’s Chief Dental Officer
Walking into a dentist’s office can sometimes feel like stepping into a world of mystery.
With all the buzzing tools, unfamiliar jargon and bright lights, it's easy to feel a bit overwhelmed. But fear not! By understanding the ins and outs of your dental visit and being equipped with the right knowledge, you can avoid unexpected costs and feel confident to ask the right questions, especially when it comes to your coverage.
Let's explore the world of dental care with a smile!
Most dentists use the annual Ontario Dental Association (ODA) Suggested Fee Guide as a reference for what they can or should charge for each service. Ultimately dental providers can set their own service fees and so charges may vary by dental provider, service or procedure.
Every year, your plan sponsor reviews the dental fee guide to understand its impact on coverage, especially when trying to manage consecutive fee increases that substantially impact the sustainability of your benefit plan.
Important reminders for a smooth visit to the dentist:
Know before you go!
Make sure you understand the details of your dental coverage before your visit by reviewing your benefits booklet available in your plan member account. This can help you prepare for any unforeseen out-of-pocket expenses.
For example, most recall exams, scaling and fluoride treatments are typically eligible for reimbursement once every six or nine months. Timing can make a big difference! Make sure you understand your dental coverage limit and when your limits are renewed.
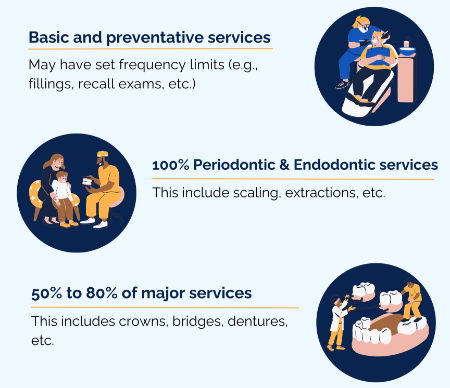
Dental coverage varies by plan. This can include different co-insurance amounts, lifetime, annual or benefit year maximums as well as the frequency of treatments that can impact the amount of reimbursement you may receive.
#ToothTruth! X-ray eligibility is based on frequency (i.e., every nine months up to 36 months) and the type of x-ray you get may have a different frequency limit compared to others. Double-check your eligibility before your appointment or treatment to avoid surprises!
Submitting an estimate
If you require major restorative work (e.g., crowns, bridges and dentures) or orthodontic treatments (e.g., braces and aligners), ask your dental provider to submit an estimate, also called a pre-determination, before agreeing to treatment or booking another appointment. You can also collect treatment information from your dentist and submit an estimate via your plan member portal.
Tip! Your dentist should always explain costs before treatment. If a procedure costs more than $300, request an estimate to make sure your treatment plan aligns with your dental benefits. Keep in mind that it may take five to 10 business days to process your pre-determination after the date received and determine whether the insurer needs more information from your dental provider.
Decoding your dental bill
Whether your treatment is fully covered by your plan or you had to pay out of pocket, always request a printed explanation of benefits after your appointment. This document breaks down what your dentist charges for each service and outlines your benefits coverage. How much they charge you and what they charge for can impact your coverage at your next visit, especially if there are frequency or unit limits.
The explanation of benefits shows:
- the service date,
- the type(s) of service(s) provided (including units of time, if applicable),
- the procedure code of each service rendered,
- the cost(s) of the service(s) charged by your dentist,
- the co-insurance (e.g., it may show 100% covered by benefits or 80 to 50% member payment required), and
- how much was covered by your benefits.
Orthodontics
Orthodontic treatments are often costly but necessary, and can pop up out of nowhere, leading to many questions.
Typically, claims for dental services are submitted after the services have been rendered; however, orthodontic treatments are an exception. Orthodontic treatments may be billed at the beginning of treatment. For example, members may be able to submit the full cost of braces at the start of treatment even if the treatment plan spans two years and includes multiple appointments.
Before agreeing to any treatment plan, always:
- Submit an estimate to understand how much you may need to pay out of pocket, depending on coverage limits.
- Confirm if your plan allows lump sum or advance payments.
- Understand how coordination of benefits (COB) works, if applicable to you.
#ToothTruth! Your orthodontist may offer the option to make lump sum or advance payments for services; however, it’s important to check how your plan reimburses orthodontic expenses. Some plans do not reimburse lump sum or advance payments but instead issue monthly or quarterly payments.
Conclusion
Dental hygiene is important, just like understanding your benefits coverage and actively participating in your dental care. Always review your benefits booklet or summary through your plan member account before booking dental appointments. When in doubt, ask your dentist to submit an estimate to confirm your treatment is covered under your benefits, helping you to avoid unexpected out-of-pocket expenses.
About Dr. Paul Bhatti
Dr. Paul Bhatti is a licensed oral and maxillofacial surgeon a fellow of the Royal College of Dentists of Canada and a Diplomate of the American Board for Oral and Maxillofacial Surgery. He joined OTIP in 2024 as Chief Dental Officer to lead OTIP’s innovative dental strategy for group benefit plan members.
and a Diplomate of the American Board for Oral and Maxillofacial Surgery. He joined OTIP in 2024 as Chief Dental Officer to lead OTIP’s innovative dental strategy for group benefit plan members.